The retina, that remarkably thin layer of specialized neural tissue lining the back inner wall of the eye, functions as the crucial image sensor, converting incoming light into electrical impulses that the brain interprets as vision. This delicate sheet is naturally secured to the underlying tissue—the retinal pigment epithelium (RPE)—which provides it with essential nourishment and oxygen. When the term “retinal detachment” is used, it describes an urgent, physically significant event where this sensory tissue is pulled away or separates from its vital underlying support structure. This separation immediately cuts off the retina’s blood supply and nutrient exchange, leading to a rapid and devastating loss of function in the affected area, much like an unplugged camera or a plant uprooted from its soil. The gravity of this condition is entirely tied to this deprivation, as the detached cells quickly cease to function, and if reattachment is not achieved quickly, the damage can become permanent. The subsequent narrative will dissect the intricate mechanics, the unmistakable warning signs, and the critical surgical interventions associated with this sight-threatening emergency.
The gravity of this condition is entirely tied to this deprivation, as the detached cells quickly cease to function
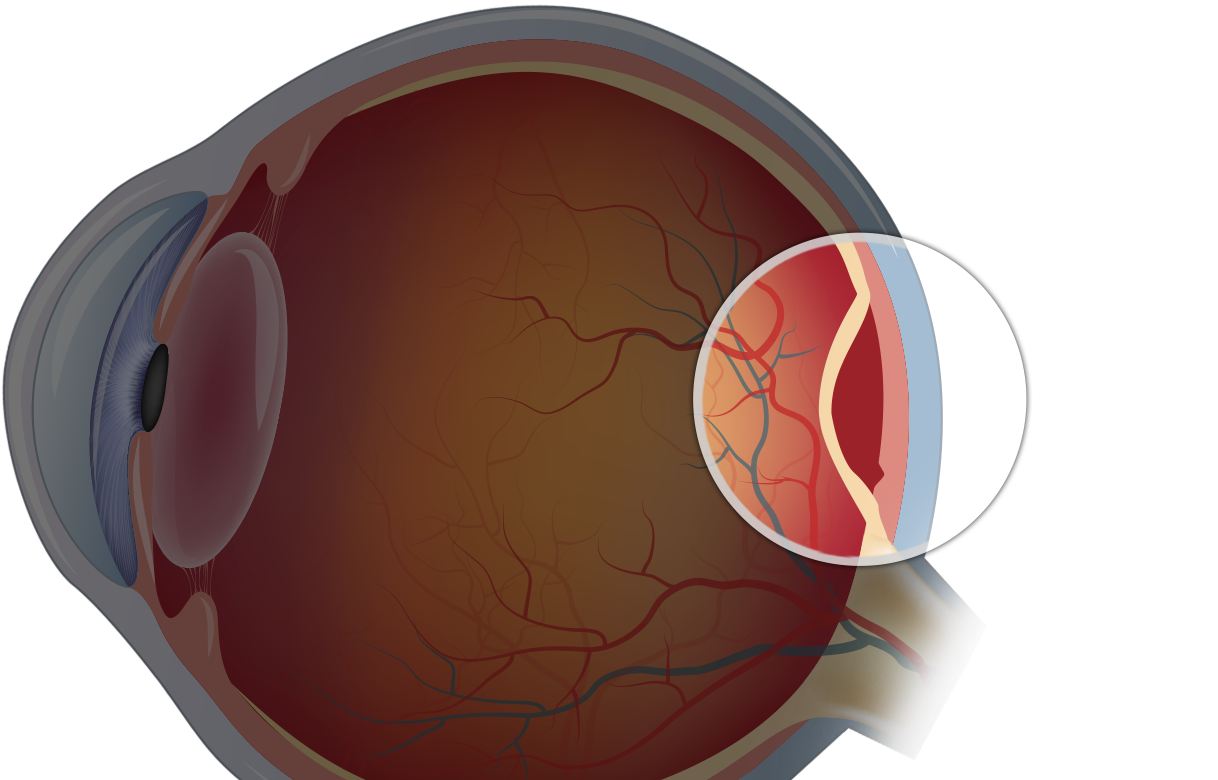
The development of a detached retina is not a singular phenomenon, but rather a cascade of distinct pathological processes. The most prevalent form is the rhegmatogenous retinal detachment (RRD), which derives its name from the Greek word rhegma, meaning a break or tear. This type begins with a physical break in the retinal tissue itself, which acts as a conduit. Liquified vitreous humor—the clear, gel-like substance that fills the main cavity of the eye—then seeps through this rent, migrating into the potential space between the sensory retina and the RPE. As more fluid accumulates, the hydrostatic pressure forces the retina to peel away, effectively stripping it from its anchor points and causing the separation to spread, analogous to wallpaper peeling away from a damp wall. These breaks are often a consequence of normal age-related changes, where the vitreous naturally shrinks and pulls away from the retina, a process known as posterior vitreous detachment (PVD). If the vitreous gel is abnormally adherent at certain spots, this pulling motion can generate sufficient force to create a tear.
A different mechanism entirely underlies tractional retinal detachment (TRD). In this scenario, there is no initial retinal break. Instead, the separation is driven by mechanical forces exerted by abnormal, contracting membranes that have formed on the surface of the retina or within the vitreous gel. These membranes, composed of scar-like fibrovascular tissue, pull and tug on the fragile retinal surface, elevating it off the RPE. The most common precursor for TRD is proliferative diabetic retinopathy, where poor blood sugar control leads to the growth of abnormal, fragile blood vessels that bleed and form scar tissue. Other causes include severe eye trauma or complications from previous eye surgeries. Management of TRD is inherently more complex, often requiring the surgical excision of this contractive scar tissue to relieve the tension and allow the retina to settle back into place.
This type begins with a physical break in the retinal tissue itself, which acts as a conduit
The third and least common category is exudative retinal detachment (ERD), also referred to as serous detachment. This type is unique in that it occurs without any tears, holes, or tractional forces. It is caused by the accumulation of fluid—an exudate—that leaks into the subretinal space from the underlying blood vessels due to inflammatory conditions, tumors, or severe systemic vascular disorders like malignant hypertension. This fluid build-up elevates the retina from below, much like a blister. Crucially, because ERD does not involve a structural break, it is often managed non-surgically by treating the underlying systemic disease—inflammation, tumor, or vascular issue—which, once resolved, allows the fluid to be reabsorbed and the retina to spontaneously reattach. Understanding these three distinct pathogeneses is vital for the ophthalmologist, as the classification dictates the correct and timely therapeutic approach.
When a retinal detachment begins, the initial visual disturbances serve as an unmistakable, though often disregarded, early warning system. These symptoms are invariably sudden in onset and typically painless, a deceptive characteristic that can sometimes delay a patient’s urgent visit to a specialist. The two most common harbingers are a sudden increase in floaters and flashes of light, known as photopsia. Floaters appear as dark specks, webs, or thread-like shapes that drift across the visual field, which are actually minute clumps of cells or debris suspended in the vitreous casting shadows on the retina. A sudden, dramatic shower of these is often indicative of the vitreous pulling away and stirring up cellular material, potentially signaling the creation of a retinal tear. The photopsia—the flashes of light—are a direct result of the vitreous pulling on the retina. Since the retina only processes light, any mechanical stimulation, such as traction, is perceived by the brain as a flicker or flash, particularly in the peripheral vision.
A sudden increase in floaters and flashes of light, known as photopsia
As the detachment progresses and involves a larger area of the retina, the symptoms escalate to a partial or total obscuration of vision. Patients frequently describe the sensation of a dark shadow or a curtain being drawn across their field of vision. This visual field loss corresponds directly to the area of the retina that has detached and ceased to function. If the detachment is peripheral, the patient may initially only notice a loss of side vision. However, if the detachment extends to the macula—the small, central part of the retina responsible for sharp, detailed central vision—the patient’s ability to read, drive, and recognize faces is immediately and severely compromised. The involvement of the macula is the defining prognostic factor for the outcome of surgery; a macula-off detachment, where the central vision is lost, carries a poorer visual prognosis even after successful reattachment.
Given the time-critical nature of the injury—where every hour of detachment contributes to irreversible retinal cell damage—treatment is almost exclusively surgical, with the objective being rapid reattachment. The choice of surgical procedure is highly dependent on the type, location, and extent of the detachment. For certain RRDs with a relatively localized, superior tear, the least invasive option is pneumatic retinopexy. This involves injecting a gas bubble into the center of the eye. The patient is then positioned so that this gas bubble floats up to physically block the retinal tear, acting as a temporary internal tamponade. The tear is then sealed with a laser (photocoagulation) or a freezing probe (cryopexy).
Patients frequently describe the sensation of a dark shadow or a curtain being drawn across their field of vision
For more complex or widespread detachments, the surgeon may opt for a scleral buckle procedure. This involves suturing a small silicone band or sponge onto the outside of the eyeball (the sclera) over the area of the tear. This band gently indents the eye wall inward, pushing the underlying RPE and choroid layers closer to the detached retina, thereby closing the tear and supporting the retina externally. The third major surgical approach is a vitrectomy, a procedure that has become the gold standard for many complex cases, especially tractional and complicated rhegmatogenous detachments. A vitrectomy involves the meticulous removal of the vitreous gel from the eye cavity, which eliminates the tractional forces that caused the detachment. Following the removal of the vitreous, the surgeon may flatten the retina and then inject a substitute material—such as an oil or gas bubble—to hold the retina in place while the tear heals, again sealing the break with laser or cryopexy.
The long-term visual prognosis following surgical repair is heavily contingent upon one critical variable: whether the macula was detached, and if so, for how long. The primary anatomical success rate for a single operation—meaning the retina is reattached after the first surgery—is high, often exceeding 90% in modern surgical centers. Even if a subsequent surgery is required, the final reattachment rate is near 100%. However, anatomical success does not automatically equate to functional visual success. If the macula was involved in the detachment, the delicate photoreceptors responsible for sharp central vision may have suffered irreparable damage from the period of oxygen deprivation. Patients with macula-off detachments often face the reality of residual visual impairment, which may manifest as persistent blurriness, distortion, or a permanent reduction in the clarity of their central vision, despite the successful surgical reattachment of the tissue. The recovery of sight, even in successful cases, can be a slow process, sometimes taking a year or more for the vision to stabilize and potentially reach its maximum level of recovery.
The long-term visual prognosis following surgical repair is heavily contingent upon one critical variable
Recognizing the various factors that heighten an individual’s susceptibility to a retinal detachment is a key component of preventative ophthalmology. The most significant and common risk factor is age, with the majority of detachments occurring in individuals over 50, a reflection of the normal, progressive changes in the vitreous humor. Another prominent factor is high myopia, or severe nearsightedness. Extremely myopic eyes are structurally longer than normal eyes, causing the retinal tissue to be abnormally stretched and thinned, making it more prone to tears and lattice degeneration—areas of peripheral retinal thinning. Furthermore, a history of previous cataract surgery or other intraocular procedures slightly increases the risk of an RRD, due to the manipulation of the eye’s internal structures during the operation. Similarly, a severe eye injury or blunt force trauma to the head or eye can directly lead to a retinal tear, as can a family history of the condition, suggesting a genetic predisposition for underlying retinal weaknesses. Awareness of these specific risk factors underscores the need for regular, comprehensive dilated eye examinations, especially in high-risk groups, to allow for the prophylactic identification and sealing of small, asymptomatic retinal tears before they progress into a full-blown detachment. The seriousness of the diagnosis demands immediate attention; the race against time to restore the retina’s connection to its life support system is the essence of this medical emergency.
The prompt, definitive intervention of an ophthalmologist is indispensable for preventing irreversible loss of sight caused by the rapid, cascading cellular damage of detachment.
